Background
Cataracts are the leading cause of blindness today, affecting 20 million people worldwide (World Health Organization). Half of Americans above 80 years old are affected by cataracts (National Eye Institute), and so are many animals! The National Eye Institute projects that in 30 years, the number of cataract patients will increase to 50 million (National Eye Institute).
What are Cataracts?
The lens is mostly made of proteins called crystallins. Crystallin proteins are normally soluble, which keeps the lens clear and allows light entering the eye to focus. When these proteins are damaged, they form insoluble clumps (Truscott, 2005). This causes the clouding seen in cataractous lenses, which scatters light and in turn makes vision blurry (Figure 1.1).

Cataracts can be caused by many factors, including radiation and diabetes, but the underlying cause is oxidative damage. Oxidative damage happens when unstable chemicals containing oxygen react with DNA, lipids, or proteins, disrupting cellular functions (Truscott, 2005). In the lens, crystallin proteins can be oxidized by hydrogen peroxide (H₂O₂), which is a reactive molecule produced during aerobic respiration (Giorgio et al., 2007). H₂O₂ reacts with protein residues and changes the shape of the protein. When two cysteine residues on separate proteins are oxidized by H₂O₂, for example, they can form a disulfide bond, which links these proteins together. The damaged proteins thus aggregate and form clumps in the lens (Truscott, 2005) (Figure 1.2).

In the eye, a natural antioxidant called glutathione (GSH) exists, which can convert H₂O₂ into water (Giblin, 2000). With age, however, GSH levels decrease, and oxidative damage caused by H₂O₂ increases. When there is more H₂O₂ in the lens than GSH can remove, crystallins become damaged (Figure 1.3). When GSH levels are low, H₂O₂ starts to oxidize crystallins and cause cataracts. As lens cells age, they move towards the nucleus and their GSH levels fall (Cvekl & Ashery-Padan, 2014), which may explain why the older cells in the lens nucleus are more prone to developing cataracts


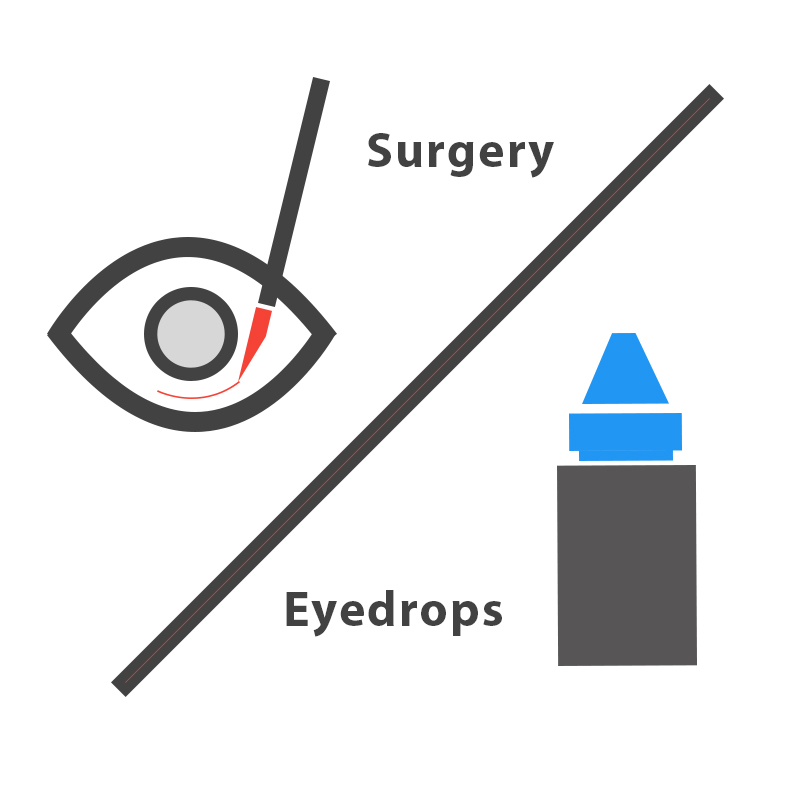
The current standard treatment for cataracts is surgery, which replaces the cloudy lens with a clear artificial lens. Surgery is effective, but like all surgeries, it is invasive and requires professional equipment and trained surgeons. These requirements add to the cost, which averages about $3,500 per eye in the US without insurance (Sigre, 2016), and is the biggest obstacle to solving cataracts worldwide. Through literature research, we found a molecule called 25-hydroxycholesterol (25HC) that can reverse protein aggregation. We hope to use this as an alternative to surgery to treat cataracts.
What is our Solution?
Our goal is to develop noninvasive, easy-to-use, and affordable eyedrops to prevent and treat cataracts (Figure 1.5).
Prevention
When GSH is present, H₂O₂ can oxidize GSH instead of crystallin proteins. When GSH becomes oxidized, a disulfide bond forms between two GSH molecules, which become oxidized glutathione (GSSG). Through literature research, we found an enzyme that recycles GSSG back into GSH. This enzyme is called glutathione reductase (GSR) (Ganea & Harding, 2006). As seen in Figure 1.6, GSR (green) recycles GSSG back into GSH, so that crystallin proteins remain protected. Even though GSR exists in the lens, its levels decrease with age, which leads to the development of cataracts (Michael & Bron, 2011). Our goal is to independently produce and deliver GSR to the lens, so that cataract formation is prevented.



Treatment
We also found a molecule that can restore solubility of protein clumps and lens transparency. It is called 25-hydroxycholesterol (25HC) (Makley et al., 2015). 25HC can be produced from cholesterol by the enzyme cholesterol 25-hydroxylase (CH25H) (Figure 1.7). Our goal is to independently produce and deliver CH25H to the lens, so that cataracts can be treated.

Citations
Cvekl, A., & Ashery-Padan, R. (2014). The cellular and molecular mechanisms of vertebrate lens development. Development, 141(23), 4432-4447.
Ganea, E. & Harding, J. J. (2006). Glutathione-related enzymes and the eye. Curr Eye Res., 31(1), 1–11
Giblin, F. J. (2000). Glutathione: a vital lens antioxidant. Journal of Ocular Pharmacology and Therapeutics, 16(2), 121-135.
Giorgio, M., Trinei, M., Migliaccio, E., & Pelicci, P. (2007). Nature Reviews Molecular Cell Biology, 8(9), 722-8.
Makley, L. N., McMenimen, K. A., DeVree, B. T., Goldman, J. W., McGlasson, B. N., Rajagopal, P., Dunyak, B.M., McQuade, T.J., Thompson, A.D., Sunahara, R., Klevit, R.E., Andley, U.P., and Gestwicki, J.E. (2015). Pharmacological chaperone for α-crystallin partially restores transparency in cataract models. Science, 350(6261), 674-677.
Michael, R., & Bron, A. J. (2011). The ageing lens and cataract: a model of normal and pathological ageing. Philosophical Transactions of the Royal Society of London B: Biological Sciences, 366(1568), 1278-1292.
National Eye Institute | Cataracts. (n.d.). Retrieved October 04, 2016, from https://nei.nih.gov/eyedata/cataract
Segre L (2016, Sept. 21). Cataract surgery cost. Retrieved from http://www.allaboutvision.com/conditions/cataract-surgery-cost.htm
Truscott, RJ (2005). Age-related nuclear cataract-oxidation is the key. Exp Eye Res., 80(5): 709-25.
World Health Organization | Priority eye diseases. (n.d.). Retrieved October 03, 2016, from http://www.who.int/blindness/causes/priority/en/index1.html

×
Zoom out to see animation.
Your screen resolution is too low unless you zoom out


