
iGEM Tel-Hai 2016
Applied design
There is no cure for Cystic Fibrosis (CF), but treatments can ease symptoms and reduce complications, and eventually destined to prolong the life expectancy.
Our project offers a new way to address the problem. We do not offer more medication to deal with the symptom but to correct the source of the disease. Our design is a single therapy, of which will be taken via inhalation directly into the lungs. This drug will repair the DNA of patients and thereby express a healthy phenotype.
Repairing the mutation in CF cells have already been done successfully with a variety of gene editing technologies in cell cultures. Moreover, a novel technology called CRISPR/Cas9 made the repair even more simple, cheap and efficient than before. These days, scientists all over the world improve the CRISPR/Cas9 technology to make it even better.
However, gene therapy depends on the ability to introduce recombinant genes into targeted cells. Gene transfer can be performed by injecting DNA into the nucleus of the cell. As a therapy this method is limited by the number of cells which can be injected and therefore inefficient. Thus, various methods were developed for introducing DNA into large population of cells [1-4]
These methods include:
- Transfection with CaPO4
- Electroporation
- Liposome fusion
- Chemically conjugated poly-lysine proteins that bind specific receptors on target cells
- DNA binding proteins genetically fused to receptor binding ligands.
These methods are limited; they require in vitro modification of the ligands using chemical or enzymatic methods in order to create a compound capable of binding DNA. Furthermore, the use of poly-lysine augments the immunogenicity of proteins. In the case of liposome fusion, systemic treatment has been found to be very limited and inefficient as liposomes accumulate in the liver [5]. CaPO4 and electroporation cannot be used as a treatment in vivo. Using DNA binding proteins is limited to direct administration into target cells since these complexes that have been used until now cannot pass the stomach or skin barriers.
Our Design
As we were looking for a novel delivery system for CRISPR/Cas9 to epithelial cell tissue (A specific tissue which is damaged by the CF mutations), we came across an article presenting a hypothesis that there is a strong correlation between CF and the Cholera disease [1], which made CF heterozygote more resistance to Cholera epidermis in the past. Therefore, giving them an advantage to survive along the years. This strong correlation leads us to investigate the mechanism of the Cholera toxin and come out with the idea of biomimicry (an approach to innovation that seeks sustainable solutions to human challenges by emulating nature's time-tested patterns and strategies). The Cholera Toxin B subunit found to be a stable, specific, efficient and non-toxic delivery system in theory [6-11].
Stable: The Cholera Toxin natural pathway occur in digestive system therefore its properties evolutionary are adjusted to extreme conditions< like pH of the digestive tract and skin barriers.
Specific: CT's natural mechanism of action occur in the digestive tract, to be more specific it occurs in the Epithelial tissue of the guts.< Therefore, the toxin is programed to bind specifically to ganglioside receptors which can be found only in Epithelial tissues.
Efficient: CT can bind to its receptor with high affinity (KD 10-10 – 10-12 M), for simplicity, it has higher affinity than an antibody to its< epitope.
Non-Toxic: The B-subunit of CT is non-toxic to human cells and is responsible only for the binding and penetration to the epithelial cells.
The following content will provide two designs for a binding method, both based on attaching CRISPR/Cas9 plasmid to the Cholera Toxin (CT) and Heat-Labile Toxin (LT), an analog of CT in E. Coli.
-
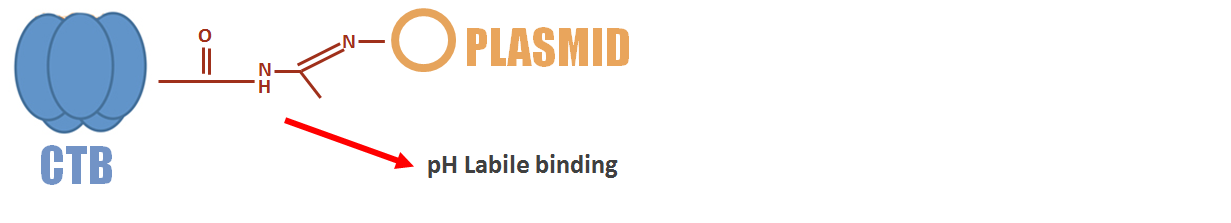
Chemical Binding - Guided by Dr. Khatib an expert on organic chemistry:
Residues of certain amino acids contain carboxylic acid that can be found in the toxin. For the first step a chemical linker 3-amino-1,2 -propanediol is attach to the carboxylic acid by nucleophilic attack reaction. Then, the toxin is oxidized and mixed with the plasmid to form an imine bond with the amine group that can be found in the plasmid's nucleotides. This bond is pH labile, meaning it can be break apart as it enters the cell and the plasmid then can go free to cell nucleus.
-
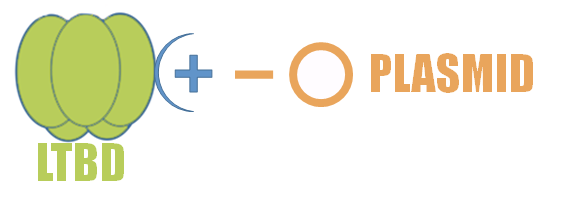
DNA Binding Domain (DBD) - Guided by Dr. Cohen-Kutner and Dr. Bachnoff
Some viruses have DBD which is a protein domain that contains a motif that recognizes ds/ssDNA. A DBD can have general affinity towards DNA or recognize a specific DNA sequence. Those proteins have a special amino acid peptide positively charge which can bind to DNA.
BBa_K2061005: Recombinant B-subunit of the E. coli Heat Labile Toxin (LTB) sequence is fused with a linker sequence and short viral DNA binding domain (DBD) sequence. This new chimeric protein (LTBD) can attach to desired CRISPR/Cas9 plasmid to be expressed in target cells
Those two delivery solutions do not apply only regarding CRISPR/Cas9 plasmids. They can be applied to a diverse of other DNA cargos such as:
- RNAi molecules
- Tumor suppressing genes
- Immunogenic epitopes in cancer therapy
The unique property of binding specifically to Epithelial tissue can lead to more therapeutics for diseases like:
- Psoriasis
- Vitiligo
- Various types of cancer
Please go to "Proof of Concept" to watch our design results.
Advanced design will occur after the progressive development of the drug. The patient will be able to take the drug in a variety of methods, depending on the disease. For example, CF patients can inhale the drug directly to the lungs and reach the cells of the airway epithelia or by swallowing pills in order to reach the gastrointestinal epithelium.
However, using CTB (or LTB) has a problem that needs to be solved: CTB is highly immunogenic and using it multiple times might cause the production of antibodies leading to an immune response.
This problem can be solved with several approaches:
- Using the drug as a single treatment.
- Using a coating molecule.
- Temporally depressing the immune system.
On the other hand, Using CTB immunogenic features can be useful in helping the immune system to recognize cancer cells and destroy them.
- Chen, C., & Okayama, H. (1987). High-efficiency transformation of mammalian cells by plasmid DNA. Molecular and cellular biology, 7(8), 2745-2752.
- Chu, G., Hayakawa, H., & Berg, P. (1987). Electroporation for the efficient transfection of mammalian cells with DNA. Nucleic acids research, 15(3), 1311-1326.
- Felgner, P. L., Gadek, T. R., Holm, M., Roman, R., Chan, H. W., Wenz, M., ... & Danielsen, M. (1987). Lipofection: a highly efficient, lipid-mediated DNA-transfection procedure. Proceedings of the National Academy of Sciences, 84(21), 7413-7417.
- Curiel, D. T., Agarwal, S., Romer, M. U., Wagner, E., Cotten, M., Birnstiel, M. L., & Boucher, R. C. (1992). Gene transfer to respiratory epithelial cells via the receptor-mediated endocytosis pathway. Am. J. Respir. Cell Mol. Biol,6, 247-252.
- Leng, Q., Woodle, M. C., Lu, P. Y., & Mixson, A. J. (2009). Advances in systemic siRNA delivery. Drugs of the future, 34(9), 721.
- Rodman, D. M., & Zamudio, S. (1991). The cystic fibrosis heterozygote—advantage in surviving cholera?. Medical hypotheses, 36(3), 253-258.
- Bharati, K., & Ganguly, N. K. (2011). Cholera toxin: a paradigm of a multifunctional protein. The Indian journal of medical research, 133(2), 179.
- Kuziemko, G. M., Stroh, M., & Stevens, R. C. (1996). Cholera toxin binding affinity and specificity for gangliosides determined by surface plasmon resonance. Biochemistry, 35(20), 6375-6384.
- Baldauf, K. J., Royal, J. M., Hamorsky, K. T., & Matoba, N. (2015). Cholera Toxin B: one subunit with many pharmaceutical applications. Toxins, 7(3), 974-996.
- Chen, C., Przedpelski, A., Tepp, W. H., Pellett, S., Johnson, E. A., & Barbieri, J. T. (2015). Heat-labile enterotoxin IIa, a platform to deliver heterologous proteins into neurons. Mbio, 6(4), e00734-15.
- 6. Spangler, B. D. (1992). Structure and function of cholera toxin and the related Escherichia coli heat-labile enterotoxin. Microbiological reviews,56(4), 622-647.

