<!DOCTYPE html>
Introduction
Mosquito-borne illnesses are responsible for the deaths of more than 725,000 people annually, ranking mosquitoes as the number one cause of animal-related deaths1. These illnesses include chikungunya virus, dengue virus, Eastern equine encephalitis, Japanese encephalitis, La Crosse encephalitis, malaria, St. Louis encephalitis, West Nile virus, yellow fever, and Zika virus2. In particular, Zika virus has been gathering much attention this year as an international health concern because pregnant women infected with Zika give birth to babies with microcephaly - a rare neurological birth defect that results in babies being born with abnormally small heads and developmental issues3. Although vaccines have been developed for certain mosquito-borne illnesses, for the most part, vaccines are not available, treatment options are limited, and there are no definitive cures3. In other words, preventing mosquito bites is the best method for dealing with mosquito-borne illnesses.

For this reason, mosquitoes repellents play a major role in mosquito-borne illness prevention (See our FAQ for more details on ways to prevent mosquito bites). Currently, the most widely used mosquito repellants are diethyltoluamide (DEET) - based because it has been proven to be effective in preventing bites from insects such as mosquitoes, biting flies, fleas, and small flying insects. Although DEET is generally safe for use at appropriate concentrations and amounts, it has been implicated in various health concerns, including: damage to DNA in laboratory animals and human cells due to the generation of free radical species, DEET crossing the placenta in pregnant lab animals and negatively affecting the nervous system and behavior of offsprings, synergisms with other pesticides, and causing rare toxic reactions when used improperly4. On top of the potential health concerns, DEET is a suspected environmental contaminants that has been implicated in harming the developing chicks of birds4 and being harmful towards fish and insects at extremely high concentrations5. It is to be noted and emphasized, however, that under proper use at concentrations designed for human use, DEET is safe for use and has been approved by the United States Environmental Agency.

The purpose of this project it to improve on available mosquito repellents by providing a natural, eco-friendly, and consumer-friendly alternative. The reason that the synthetic DEET compound is used so widely is because of its comparatively long effectiveness compared to natural alternatives such as citronella oil and p-menthane-3,-8-diol (PMD). In order to resolve this issue regarding duration of efficacy, we are developing genetically engineered microbes that release rhamnolipids, a commonly used biosurfactant which has been shown to effectively repel mosquitoes. By applying these engineered microbes to the skin via a lotion, we hope to provide a long-lasting mosquito repellent superior to synthetically produced repellents like DEET.
Rhamnolipids repel Aedes aegypti mosquitos
In order to quantify how effectively rhamnolipids repel mosquitoes, we conducted mosquito feeding and landing assays. Aedes aegypti, the species of mosquito observed to carry Zika virus, were grown from larval stage, and females were sorted at the pupae or adult stage. Since only females consume blood for reproduction, we were only interested in using them for the assays.
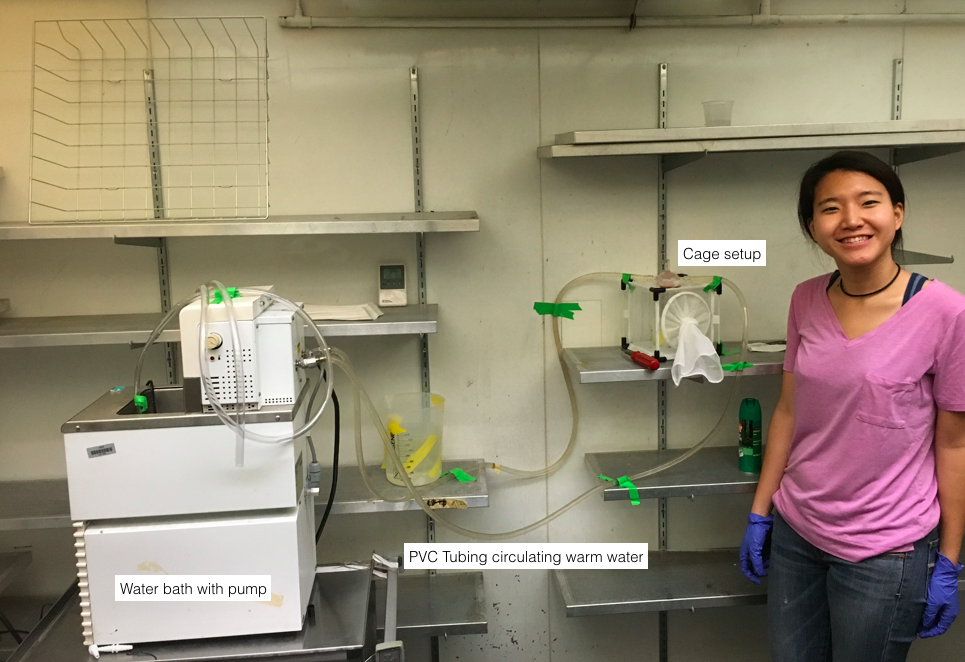

One day before experiment, 50 total mosquitos (with 30 females) were isolated in cages and starved from 23-25 hours. Each cage was then taken to a warm room (~30 °C), and the cage was covered with wet paper towels to preserve humidity. For each trial, our blood feeding system (Figure) was placed on top of the cage each with a cotton gauze soaked with either negative control water, 1 mg/mL mono-rhamnolipid solution, 1 mg/mL di-rhamnolipid solution, or positive control 25% DEET, and the mosquito activity was videotaped for 1 hour. Afterwards, the cage was taken to the cold room to paralyze the assayed mosquitoes, and mosquitoes that had consumed blood were counted. It is important to note that the age of female mosquitoes and the time of feeding played an important role in how mosquitoes behave. Typically, it is optimum to use female mosquitoes of age from 4-6 days for feeding assays as any mosquitoes older than this age range will be too old to reproduce, and thereby not needing to drink blood. Furthermore, their feeding is most active 4 hours before dusk. Some of our trials that didn’t meet these criteria did not result in any feeding, but we did observe significant difference in landing between the control and rhamnolipids. Our landing assay results showed that while DEET was the strongest mosquito repellent with no landings or fed mosquitos, 1 mg/mL mono and di-rhamnolipid still showed statistically significant repulsion as shown in the graph below.

P. putida, S. epidermidis, and rhamnolipids are compatible with human keratinocytes
Determination of rhamnolipid IC50

Keratinocytes, human skin cells, were grown for several days. When the cells were 80% confluent, they were seeded in 24 well plates at a density of 2.5105. The cells were weaned off of antibiotics the following day before they were treated with varying concentrations of rhamnolipids and the reagent MTS. The MTS assay reveals the cell viability of the cells. Using this information, the data was normalized and statistically analyzed to determine the keratinocyte IC50—or the concentration of rhamnolipid that induces 50% cell death. The IC50 was determined to be between 45.19 µ/mL and 65.52 µ/mL. Relating the results to rhamnolipid quantification, the concentration of rhamnolipid the construct produces should not cause significant cell death.
Keratinocyte cell viability bacteria assay

Keratinocytes were co-cultured with different strains of bacteria (Pseudomonas putida, Pseudomonas aeruginosa PAK, Staphylococcus aureus, Staphylococcus epidermidis, and mutant rhlAB P. putida). Half were cultured in plain DMEM with serum, and half were culture in DMEM with 1 mg/mL mixed mono- and di- rhamnolipids. After co-culturing, the keratinocytes were washed with PBS, exposed to gentamicin in an attempt to kill the bacteria, and incubated in MTS cell viability assay for up to 4 hours and viewed in a plate reader. MTS assay is colorimetric cell viability assay and reacts with NADPH-dependent dehydrogenase enzymes, which are only active in live (metabolically active) cells6. For the MTS assay, pure media were used as a negative control (100% cell death), and keratinocyte culture with normal DMEM was used as a positive control (“0%” cell death, or the maximum number of cells that could be alive).

We originally tried to do plating experiments to see if keratinocytes internalized any bacteria, but were unable to completely kill off all the bacteria in the keratinocyte supernatant even at extremely high gentamicin concentrations and thus could not get an accurate read.
The results indicate that there is no consistent trend regarding the addition of rhamnolipid and cell viability. Rhamnolipids did not significantly increase or decrease cell viability regardless of the bacteria type as shown in the first figure since the error bars overlap. We hypothesized that the concentration of P. putida would not influence cell viability as it is an environmental strain not nearly as potent as other bacterial strains such as Pseudomonas aeruginosa PAK. As depicted in the second figure, all MOIs (ranging from 0 to 20) did not significantly influence the cell viability of the strain as shown by the overlapping error bars in the graph. These results overall indicate that our construct may not cause significant cell death once applied to the skin in an acute setting of a few hours.
Mutant rhlAB P. putida
produces rhamnolipids
Transformation of P. putida KT2440
In order to avoid the virulence factors of Pseudomonas aeruginosa, bacterial strains with similar or shared metabolic pathways to the one above were chosen as potential candidates. The final candidates were Pseudomonas putida and Staphylococcus epidermidis. Although S. epidermidis doesn’t share the same exact pathway as P. aeruginosa, it is a naturally-occurring skin microbiome and only need two additional enzymes, RhlA and RhlB, to produce mono-rhamnolipids. Genes rhlA and rhlB necessary for mono-rhamnolipid synthesis were extracted from the P. aeruginosa P14 bacterial strain. These genes were cloned into the modified plasmid pNJ3.1 using standard cloning methods for transformation into the desired bacterial strains (Figure 2). The plasmid pC194 and a shuttle vector strain, S. aureus RN4220 (details on S. epidermidis transformation are discussed in the experiments and result section) were used for S. epidermidis transformations with the same basic design (Figure 3). The conversion of mono-rhamnolipids to di-rhamnolipids requires the additional gene rhlC, which was also extracted from P14 strain and cloned into the same pNJ3.1 vector (Figure 4).
Quantification of rhamnolipids
To confirm the presence of rhamnolipids produced by our mutant strains (P. putida, E. coli transformed with pNJ3.1_rhlAB), we explored three different methods: cetyl trimethylammonium bromide agar plating (CTAB), thin-layer chromatography (TLC), and supercritical fluid chromatography mass spectrometry (SFC-MS). For TLC and SFC-MS analysis, rhamnolipids were extracted from cell culture supernatant through liquid-liquid extraction with ethyl acetate and redissolved in methanol prior to measurement. Detailed protocols on the extraction is discussed under protocols.
Cetyl trimethylammonium bromide agar plate assay

Cetyl trimethylammonium bromide (CTAB) agar plates detect the presence of rhamnolipid by reacting with the sugar in rhamnolipids7. When rhamnolipid is present, it forms blue halos around the compound, and the halo size usually correlates to the amount of rhamnolipids7. We tested this method with 95% pure rhamnolipids (Sigma-Aldrich) by plating different concentrations of the compound dissolved in water onto SW agar plate*. Blue halos were present after incubating the plate for 24 hours at 37°C, but the limit of detection was too high (~1g/L). Furthermore, depending on the amount of CTAB used per plate, the size of halos varied, which made it difficult for us to use this method as a quantitative measurement.
Thin-layer chromatography
Thin-layer chromatography (TLC) was used as a more reliable method of detecting rhamnolipids. TLC is a very common separation technique used to isolate a desired compound from a mixture. It typically involves two different phases, stationary and mobile, in which the mobile phase flows through the stationary phase and carries the components of the mixture with it8. Separation of compounds is based on the affinity of the compound towards the stationary phase vs. the mobile phase, and depending on which phase the compounds prefer, they travel with the solvent at different rates8. We used silica gel as the stationary phase and solvent consisted of chloroform, methanol, and acetic acid in 65:15:2 % volume ratio as the mobile phase. Knowing that di-rhamnolipids have more hydroxyl groups, we predicted it to have a smaller retention factor than mono-rhamnolipids as they would prefer to stay on polar silica gel. To visualize the plate, the silica gel plate was stained with four different dyes: CAM, KMnO4, orcinol with 50% H2SO4, and orcinol with 10% H2SO4. Among the four staining methods, orcinol with 10% gave the best visibility. The chemical mechanism in which orcinol and sulfuric acid react with rhamnose to create a dye is illustrated in Figure 2.

We confirmed that TLC method shows two distinct bands for mono-rhamnolipids and di-rhamnolipids, and that it has a limit of detection lower than CTAB (approximately 0.5 mg/mL). Next, we tested our mutant P. putida and E. coli strains with promoters of different strengths. For positive controls, WT P. aeruginosa and mutant P. aeruginosa were used, and for a negative control, WT P. putida was tested. When the cells were grown in LB only media, none of the rhamnolipids was detected from P. putida or E. coli. However, when the cells were grown in LB supplemented with glucose, a faint band for mono-rhamnolipids was detected from mutant E. coli transformed with a high expression level promoter. Although our construct in P. putida didn’t show any clear band, mutant P. aeruginosa transformed with the same construct showed to produce a lot more mono-rhamnolipids compared to WT P. aeruginosa, which mainly produces di-rhamnolipids. This result confirms that our construct is working as expected, yet we need a detection method with higher sensitivity.

Supercritical fluid chromatography
In order to accurately measure the amount of rhamnolipids produced by our mutant strains, we used supercritical fluid chromatography (SFC-MS). First, a test run was executed with a mixture of mono-rhamnolipids and di-rhamnolipids at the concentration of 5 mg/mL by running the sample through the column packed with 2-PIC. From this test run, we have obtained the retention times of mono-rhamnolipids (rha-C10-C10: pseudomolecular ion of 503.56 m/z) and di-rhamnolipids (rha-rha-C10-C10: pseudomolecular ion of 649.8 m/z) to be approximately 3.974 min and 4.942 min respectively. Then, a calibration curve was constructed with 95% pure mono-rhamnolipids, and the limit of detection was found to be approximately 5 µ/mL. The mass fractions were obtained from electrospray ionization (ESI) negative mode.

From our TLC analysis, it was found that supplementing the LB media with glucose is crucial to the production of rhamnolipid. Therefore, for SFC-MS analysis, all the mutant strains (E. Coli_RhlAB, E. Coli_L1_RhlAB, and P. putida_L1_RhlAB) were grown in LB supplemented with glucose. From the SFC-MS data, it was found that mutant E. coli strain makes more mono-rhamnolipids than mutant P. putida. Furthermore, the promoter strength was confirmed as expected since the mutant E. coli strain transformed with a high expression level promoter H2 produced almost 6 times more rha-C10-C10.

In order to investigate the optimum growth conditions for rhamnolipid by the mutant P. putida strain, the amount of glucose added and the time of growth were varied. Using the calibration curve above, we were able to measure the accurate amount of rhamnolipids produced in each cell culture. From this data, we have concluded that P. putida produces the most mono-rhamnolipids when grown for 24 hours in the media LB supplemented with 50 g/L of glucose.
We have also tested the mutant strain of S. aureus RN4220, the strain that carries shuttle vector for S. epidermidis. Unfortunately, SFC-MS data didn't show any production of rhamnolipids from S. aureus strain.

In order to investigate the amount of di-rhamnolipids produced, we have tested our mutant strains of P. putida transformed with rhlC gene. It was grown under the same condition of 24 hours incubation in LB media supplemented by 50 g/L of glucose. Approximately 142 µ/mL of rha-C10-C10 and 3.524 µ/mL of rha-rha-C10-C10 were detected.
Freeze-drying is a viable method
for P. putida storage
Since our product is designed to be eventually applied for every-day use, it therefore must be commercially viable, and a key to its commercial value is shelf life. Freezing is the usual treatment of commercially available products containing live bacterial culture; however, the associated cost is rather high and would render our product uncompetitive relative to existing products if freezing were the storage method chosen. Exploring other options, we decided to try freeze-drying, which is most commonly employed to treat bacteria for probiotic products. A huge advantage of the method is that freeze-dried bacteria can be stored at room temperature, which would drastically reduce the storage cost of the product and make the product accessible to many underdeveloped countries where mosquito-repellent is especially needed. The method manipulates pressure and temperature conditions so that water molecules within the cell undergo sublimation, preserving cellular integrity and properties.

Nevertheless, the existing snap-freeze protocols are mostly designed for common lab strains such as E. coli, so we experimented with different formulations for the lyoprotectant and rehydration media to optimize the protocol and to maximize post-freeze-dry survival rate for P. putida. Briefly, cells were grown to desired turbidity, collected, and washed. Pellets are resuspended in lyoprotectant containing 10% sucrose w/ LB and stored in -20 °C until frozen. Frozen samples are then incubated in liquid nitrogen to further reduce the temperature and freeze-dried in a lyophilizer for 24 hours. Samples are subsequently collected, sealed with parafilm, and stored in a dessicator. To rehydrate, Rehydration media (LB) is added to dried samples and the liquid rehydration culture is incubated at room temperature for 40 minutes.
To test the relationship between storage time and survival rate, we freeze-dried cells from the same liquid culture and rehydrated them at different time points to observe change in viable cell concentration over time. The result is shown in Figure.

Additionally, it was found that the survival rate for snap-freeze is still much higher than than that of freeze-dry; about 72% of P. putida survived after the time point of 28 days. Although the survival rate dropped to nearly zero after 28 days, there is still a considerable amount of bacteria left (~104 CFU/ml) that could potentially reproduce and secrete rhamnolipid. These results could perhaps be improved with more specialized lyophilizer since the one we had available was mainly for chemical use. Moreover, we could also potentially improve the result with a more advanced moisture-control method such as air-tight sealing.
Discussion
Overall, the team was successful in engineering a harmless strain of bacteria that can secrete rhamnolipids as a means to prevent mosquito bites. Rhamnolipid quantification assays indicated that while the construct does produce rhamnolipids, the amount must be amplified in order to ensure complete protection from mosquitoes. Mosquito experiments demonstrated that once the concentration is elevated mosquitoes will be repelled by the rhamnolipids produced by the team's construct.
Regarding safety, rhamnolipid survival assays show that Rhamnolipid will not severely affect the growth of skin bacteria such as S. epidermidis and S. aureus. Staphylococcus transformation was attempted and would have been a more permanent solution for Rhamnolipid productions, since S. epidermidis is a natural 70% coloniser of human skin. Keratinocytes experiments revealed that safety is not a prominent worry as rhamnolipids did not significantly cause cell death of healthy human skin cells in an acute setting nor did high concentration of bacteria cause significant cell death. Mouse experiments were planned and will be the final stage of safety procedures after optimizing rhamnolipid production by the bacteria construct.
Several experiments were conducted to assess the sustainability of our product or potential shelf-life if it is commercialized as a legitimate lotion. Freeze-dry versus snap freeze comparisons show that snap freeze is more effective at maintaining long-term bacterial survival, but freeze-dry maintains its position as the more practical preservation method given it needs only a desiccator as opposed to a -80 °C freezer for transport. Consequently, future experiments can be done to tweak the protocol and/or lyoprotectant to improve survival rates for consistent rhamnolipid production levels.
1 Gates, Bill. "The Deadliest Animal in the World." Gates Notes. The Gates Notes LLC, 25 April 2014. Web. 2 September 2016.
2 "Mosquito-Borne Disease." Mosquito. American Mosquito Control Association®, n.d. Web. 2 September 2016.
3 "Mosquito Diseases." Mosquito World. Mosquito World, n.d. Web. 9 September 2016.
4 "Is DEET Safe?" Bug-Off. Bug-Off, n.d. Web. 18 October 2016.
5 "DEET: General Fact Sheet." Oregon State University. National Pesticide Information Center. July 2008. Web. 18 October 2016.
6 "MTS Cell Proliferation Colorimetric Assay Kit." BioVision. Web.
7 Pinzon, Neissa M., and Lu-Kwang Ju. "Improved detection of rhamnolipid production using agar plates containing methylene blue and cetyl trimethylammonium bromide." Biotechnology Letters 31.10 (2009): 1583-588. Web.
8 Clark, Jim. "Thin Layer Chromatography." Chemguide. Web. 15 October 2016.


